Task performance by the National Health Fund in 2019
The National Health Fund discharged most of its statutory tasks in 2019 but it helped improve availability of some health services only. The waiting time for some medical procedures has shortened but the availability of outpatient specialist care has got worse. The share of ambulatory treatment is still too small when compared with hospital treatment.
In 2019, the National Health Fund (NHF) discharged its statutory tasks, not always properly, though.
The National Health Fund, which was established in 2003, has the third largest budget of all public institutions in Poland, after the Polish State and the Social Insurance Institution (ZUS). Its share in public spending on healthcare is 85%. As a powerful payer it impacts the quality and availability of medical services and is therefore obliged to analyse the structure of those costs. That imposes special requirements on the NHF in terms of managing the public funds at its disposal.
In 2019, the NHF purchased health services for over PLN 90 billion, which is over PLN 9 billion (11.2%) more than last year. That increase which has continued for yet another year made it possible to reduce the number of queuing patients- but it was not the case for all health services.
The audit also revealed that as much as 7.4% of the costs of services were expenditures for extra remuneration for medical staff (over PLN 6.5 billion). Their share in the total NHF expenditures went up disproportionately - over four times faster than the share of total costs of health services (45.5% against 11.2% correspondingly). NIK has stressed that the failure to recognise extra remuneration in the service price decreases the NHF revenue for health services provided under the coordination laws.
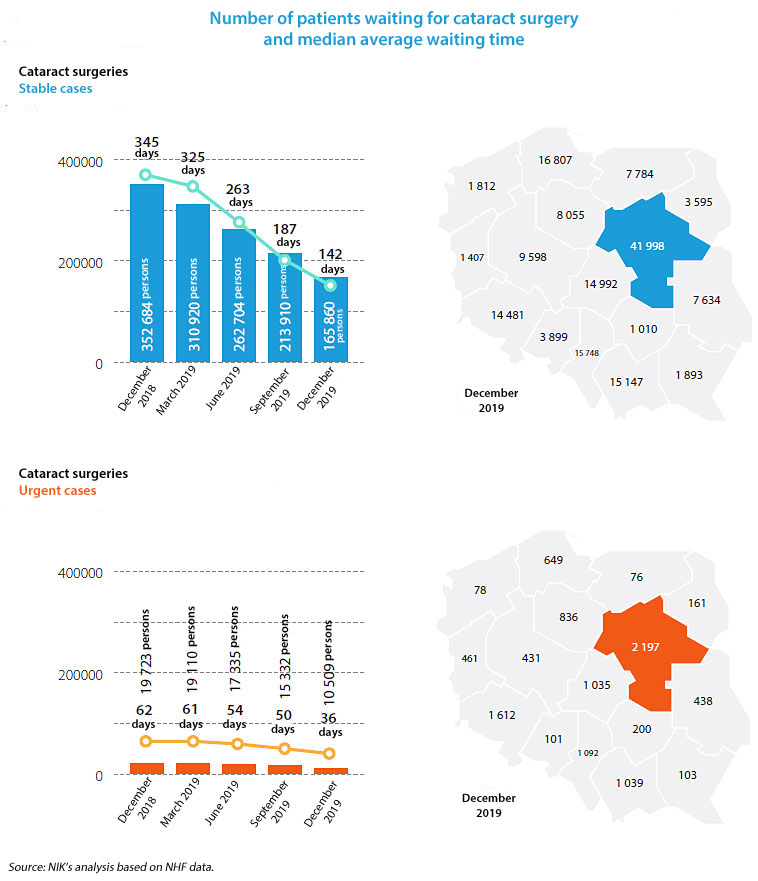
The NHF extended the list of health services covered by unlimited financing to include diagnostic imaging and cataract surgeries. The Fund also increased the subsidy for the hip and knee joint alloplasty. As a result, the number of those services went up and the queues were shortened. The best effects could be observed in case of the cataract surgeries where the waiting time was shortened by 203 days (53% decrease).
At the same time, NIK has underlined that the biggest share of the services’ costs were the hospital treatment costs (their share went up by 0.2 percentage point and totalled 52.6% in 2019). It means that the hospital treatment, which is more expensive, is more popular than the outpatient specialist care. In the opinion of NIK this is a structural irregularity. The outpatient specialist care was not properly subsidised and the waiting time in this area increased for nearly 60% of health services and the number of people waiting went up by over 15%.
In mental health care and addiction treatment the number of patients waiting for health services increased by more than 32%.
Only15.5% of eligible patients took benefit of the comprehensive medical care for patients after heart attack and 8% had cardiological rehabilitation as part of that care. At the end of 2019, comprehensive care of that type was still not available to patients in two Polish provinces.
The cardiological rehabilitation helped reduce the death rate among patients. That is why, NIK suggested that the comprehensive medical care for patients after heart attack should be made more available.
One of the key causes of long queues were missed appointments. In 2019, only in cardiological, oncological, orthopaedic and endocrinologic outpatient clinics, more than 200 thousand patients missed their appointments. The NHF tried to provide reliable and complete data about the waiting lists. It failed to launch the appointment reminder service within the statutory deadline, though.
Besides, the NHF Head Office did not exercise proper supervision over the Fund’s provincial branches in terms of preparing the healthcare purchase plans. Also, irrespective of the postulates to standardise the process of preparing the purchase plans by provincial branches, no uniform methodology has been implemented. Moreover, the provincial branches were not provided with standardised epidemiological data being the basis for planning.
The NHF introduced correction factors with regard to financing health services but it failed to analyse needs against targets. It also did not define requirements for service providers as to the quality and availability of services. This is not a positive phenomenon, according to NIK. An increase in outlays for healthcare has to go hand in hand with the care about the purpose and economy of spending.
The Fund’s financial plan was developed and executed in line with the effective law. No costs were exceeded. Despite the revenue growth, the NHF posted a loss of nearly PLN 1 billion in 2019.
The NHF’s administrative costs went up a bit more (11.7%) than the task performance costs (11%). The share of administrative costs in the total costs, as in the previous years, was small and totalled 0.8%, despite the fact that the key category, i.e. the salary costs, went up by 13.3%.
NIK has positively evaluated the decrease in the amount of non-financed costs of health services provided above the limits set in the contracts. The amount of services exceeding the limit and not recognised in the Fund’s ledgers as of their closure date totalled more than PLN 433.3 million and was 32.4% smaller than last year. At the same time, NIK pointed out that the financing of health services for patients with mechanical ventilation was not tailored to the patients’ needs. The amounts of overprovided services in that area have gone up significantly in the past four years. Only half of the Fund’s provincial branches financed all health services as of the ledgers closing date for 2019.
Until the end of the audit, the report on the execution of the Fund’s financial plan for 2019 was not approved. The NHF Council should adopt the report within 15 days of its receipt. On 23 March 2020, the term of the NHF Council expired and the new Council was not founded before the end of the audit. It was established by the Minister of Health only on 27 July 2020.
The NHF’s periodic report for 4Q2019 was not developed properly: statistic tables about provided health services are incoherent, they also contain errors or are incomplete.
The work plan of the NHF Head Office was supposed to be one of the management control tools. It did not help perform the tasks, though, as it was prepared with delay and did not cover the whole year. Besides, the plan provided neither managers nor employees with reliable information essential for task performance or objective evaluation of the target achievement level. Out of 44 projects indicated for implementation in 2019, in the work plan of the NHF Head Office, less than a half (20) was implemented in the scheduled deadline.
Recommendations
According to NIK the NHF President should take the following actions:
- analyse the increasing number of patients waiting for oncology services in the outpatient specialist care and take measures based on that analysis to curb that increase,
- boost availability of the comprehensive medical care for patients after heart attack, in particular in provinces where it was not provided before,
- take efforts to make sure that the reimbursement of costs for provided health services includes the costs of extra remuneration for medical staff,
- ensure credibility and reliability of data in periodic reports,
- implement the system of defining targets to specify the correction factors and evaluate the effects of their implementation,
- consider the management control standards for the public sector finance entities while developing and implementing the NHF work plan.


