In Poland, as in other countries, a lot of women experience miscarriages and stillbirths. According to a UNICEF report, every 16 seconds a dead baby is born somewhere around the globe. Poland and the whole Europe are located in the zone where the stillbirth ratio does not exceed 6 deaths in 1000 deliveries. In Poland it is slightly more than 3 dead babies in 1000 deliveries, similarly to Belgium, France or Hungary. There are fewer stillbirths in Czech Republic, Germany, Sweden and Finland.
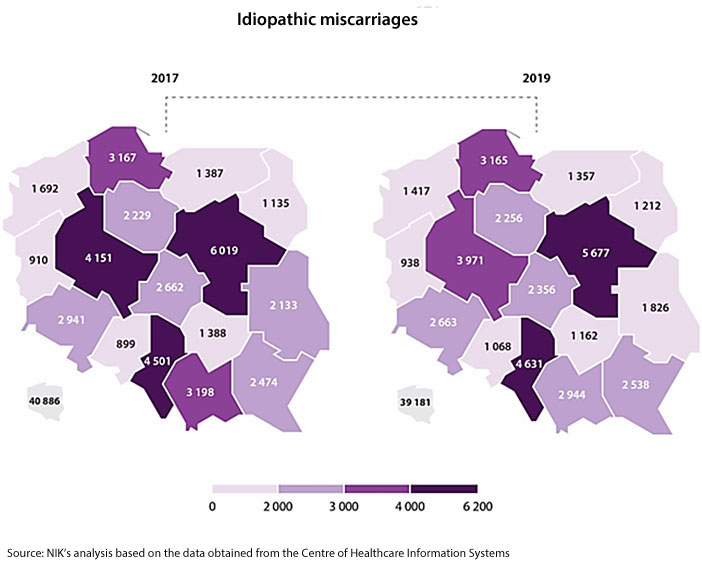
In Poland in 2017-2019, every year about 1700 women gave birth to a dead baby, whereas in about 40 thousand women the pregnancy ended in miscarriage. According to estimates, about 10-15 percent of all pregnancies result in miscarriage.

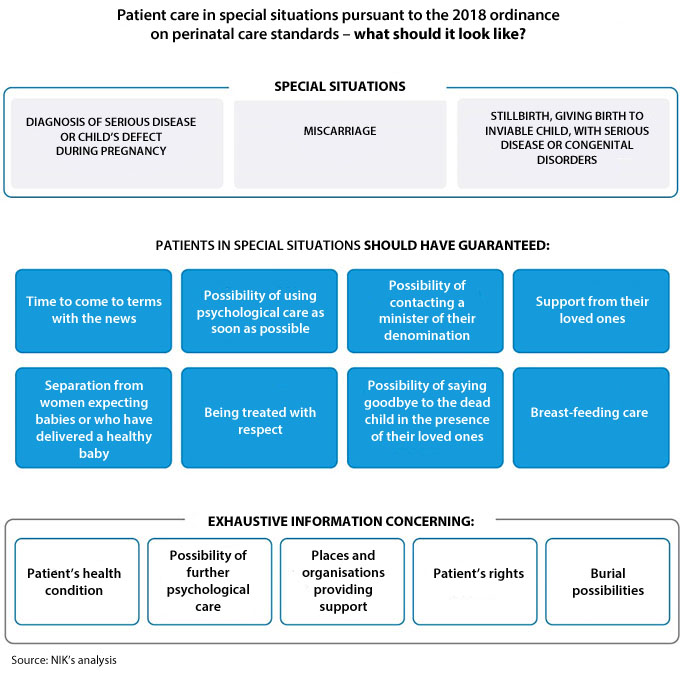
For parents these are very difficult situations. That is why, they need special care - from their environment, from their loved ones but also from medical staff taking care of them. Experience, knowledge, professionalism and interpersonal skills are essential to help such patients effectively in those dramatic situations. Medical personnel should undergo special courses and training programmes on how to handle obstetrical failures and cooperate with patients who are going through baby loss. Guidelines on taking care of such patients have been set out mainly in the ordinance of the Minister of Health of 2018 on perinatal care standards.
NIK’s audit focused on hospital care of patients who had miscarriage or stillbirth. The audit covered 37 hospitals in 7 provinces.
Audit findings
In the hospitals audited by NIK, patients who had miscarriage, stillbirth or whose baby died at birth, were not provided with adequate and sufficient care. The main reason was improper organisation of the entire process of treating such patients as well as non-compliance with applicable laws, including perinatal care standards.
Medical documentation of patients in over a half of the audited hospitals (57%) was not kept with due diligence and did not allow establishing if medical care services were provided to them in line with all effective standards.
Patient care
The care of patients experiencing miscarriage or stillbirth was often limited to essential medical services, without providing broader support. Hospital directors as well as medical staff not always noticed the need for specific care in such cases. In many situations hospital personnel simply could not talk to women who lost their babies. Working in such emotionally difficult conditions requires additional assistance. NIK’s audit showed that doctors, midwives and nurses in many hospitals lacked adequate and sufficient training programmes and advice on stress management in such situations. Both the midwives and doctors when asked about issues and needs related to patient care in case of miscarriage or stillbirth, pointed to the need for communication skills training.
It happened that medical staff simply lacked empathy. In one of the audited hospitals, patients who lost their pregnancies were given a brochure on breastfeeding and related dietary recommendations which could have deepened their baby loss trauma.
According to the President of the Childbirth with Dignity Foundation, women contacting the Foundation point to numerous problems arising mainly from the lack of preparation of some part of medical personnel and hospitals to care about women in special situations. In this way they also fail to comply with the ordinance of the Minister of Health of 2018 on perinatal care standards. The most frequently reported issue was the lack of empathy on part of medical personnel, inability to communicate with persons in extremely difficult life situations. Women underline the attitude of medical staff who tend to be impolite, arrogant, cold and ignoring. A lot of women described situations where medical personnel raised their voices at them in case they were crying or inquired about their condition.
The Association for Medical Education ”Asklepios” reported that most complaints of patients who experienced an obstetrical failure were related to improper communication between patients and medical personnel. ”Unfortunately, medical personnel often cannot talk to patients who lost their babies. This is confirmed by midwives who are willing to undergo psychological training. They want to help but often don’t know how. The fact that medical staff do not communicate properly with patients does not result from their malevolence but simply from the lack of solid preparation.”
NIK has also underlined that in nearly half of the audited hospitals, the furnishing and equipment in labour wards, sickrooms and diagnosis rooms in obstetrics and gynaecology (ob-gyn) wards did not always meet legal requirements. The organisation of labour rooms and examination rooms in four hospitals did not cater for patient rights to privacy and dignity. For instance, procedure rooms were not secured against the access of third parties and the gynecological chair was not covered from the side of the room entry.
Not in all hospitals the women who lost their babies were separated from patients expecting birth of a healthy baby or patients who delivered a healthy baby. In 5 of 14 audited hospitals, all those patients stayed in the same room. This may have an adverse impact on woman’s mental condition after a baby loss. In one hospital women after miscarriage were hospitalised in the ward corridor.
None of the audited hospitals had a separate room to say goodbye to the diseased child. Usually patients had a chance to do it in a single room where they stayed or delivered the baby.
Psychological care
Not all patients had a chance to use support of a psychologist. The scale of such assistance varied: in three audited hospitals psychological advice was not provided at all and in one hospital as much as 85% of patients used this kind of support. Most patients received psychological aid in those hospitals where a psychologist was hired in an ob-gyn ward. The problem is that the requirement to hire a psychologist for at least 0.5 FTE is valid only for the largest ob-gyn wards (level 3) which handle the most severe cases. However, despite the requirement, a psychologist was not always there in the audited ob-gyn wards. Doctors and hospital directors themselves admit that they feel the deficit of psychologists in their wards but they cannot employ those specialists.
The lack of permanent psychological care in case of patients experiencing obstetrical failures was the most common problem indicated by provincial consultants in obstetrics and gynaecology.
NIK established that in eight hospitals badly organised work of psychologists made it impossible to use their consultations. For instance, patients could not use psychological advice at weekends, on bank holidays or in the afternoons. It happened that when a psychologist appeared in the ob-gyn ward, the patients who needed psychological assistance, were not there anymore as they had already been discharged.
Most of the audited hospitals did not take all endeavours to provide psychological care to all interested patients. Also, most of the hospitals did not document properly if each patient experiencing an obstetrical failure could use psychological assistance in the shortest time possible. In 28 of 37 audited hospitals, it was not noted in the medical documentation if the given patient was informed about the possibility of using psychological care and if she declined this kind of support. The absence of such information makes it impossible to assess if that standard is met in the given hospital.
An anonymous survey made in the course of the audit among patients hospitalised due to baby loss revealed that nearly 35% of women were left without psychological care.
Headcount of doctors
In many hospitals (about 70 percent) the shortage of doctors was an issue in ob-gyn wards. Admittedly, the number of hired doctors in all the audited ob-gyn wards was consistent with legal requirements but in some hospitals it was not enough to meet the demand. As a consequence, in two of 37 audited hospitals (5%) it happened that doctors without required specialty were on unsupervised duty in ob-gyn wards.
In five hospitals (14%), doctors were not provided with the minimum of 11 hours of uninterrupted rest after the end of their shift. In one hospital, doctors documented working in the outpatient clinic and in the ward at the same time. In most of the audited hospitals (25, that is 68%) it happened that doctors employed under civil law agreements performed their work ceaselessly for over 24 hours, often on shifts exceeding 48 hours, in some cases even 88 hours. NIK stands in a position that in view of the above the quality of medical services may be questionable, not to mention the health safety of patients and doctors.
Post-miscarriage procedures
Procedures used by the audited hospitals in terms of handling bodies of miscarried and stillborn babies were not always compliant with the law. The process was not properly documented.
According to NIK, a standardised procedure is missing in all hospitals as regards patients’ declarations about handling the child’s body - decision to use or give up the right to burial. In as much as 26% of the audited hospitals the medical documentation lacked the patient’s decision in that matter. As a consequence, in five hospitals which did not have that document, the bodies of miscarried and stillborn babies were stored for a long time - in an extreme case it was six years.
There were different templates of declarations on the child’s body handling. In several cases they were incorrect and could have misled patients, thus making the child’s burial impossible.
In more than a half of the audited hospitals (19), NIK identified irregularities in the management of miscarried and stillborn children’s bodies. Six hospitals transferred children’s bodies for histopathological examination to external companies, without demanding their return. As a result, the burial of children’s bodies was impossible and in a half of the analysed cases ended in the bodies’ disposal at the order of companies making the examinations. In two hospitals, the bodies of stillborn babies were qualified as medical waste and directed for disposal.
Recommendations
To the Minister of Health to change:
- ordinance on guaranteed medical care in hospital treatment by introducing an obligation to hire a psychologist for at least 0.5 FTE in level 1 and 2 ob-gyn wards;
- ordinance on the types, scope and templates of medical documentation and the way of its processing by introducing a template of the declaration for patients who experienced miscarriage or stillbirth, documenting their decision to use the right to the child’s burial or give up that right and the obligation to attach that declaration to individual medical documentation.
NIK also recommends that the Minister of Health should take efforts to ensure standardised and legal practice of hospitals for handling the bodies of miscarried and stillborn babies.
Some recommendations were addressed to hospital directors:
- to eliminate cases of doctors’ overly long work shifts (even a few days, without any break) employed under civil law agreements. The point is to guarantee proper quality of medical care and increase patients’ safety;
- to organise training programmes for doctors and midwives on patient care in special obstetrical circumstances, covering mainly patient communication skills;
- to organise stress management support for medical personnel who care about patients in special situations;
- to keep medical documentation of patients in accordance with applicable law, including information on medical care services provided to them, in a way guaranteeing the right to information about the patient’s health condition;
- to eliminate cases of such handling of stillborn children’s bodies which prevents their burial.


