The State Medical Rescue System was designed to provide medical assistance to persons with health emergencies. Provisions governing the system organisation and principles of its operation and financing were changed many times. The last significant law changes that were to streamline the entire system operation were implemented in May 2018. The changes covered, among others, elimination of private entities having their own ambulances from the State Medical Rescue System and implementation of triage in accident and emergency departments (AEDs).
Key audit findings
Despite implemented changes and attempts to reorganise the State Medical Rescue System (SMRS) and increased expenditures on its operation, the most critical, long-time issues have not been eliminated. According to NIK, in 2018-2019 the Minister of Health and governors responsible for the system organisation, coordination and supervision, failed to provide required conditions for the system to operate efficiently.
First of all, the Minister of Health issued executive acts to the amended SMR Act with several months’ delay. The regulations were of key importance for the medical rescue system as they defined standard procedures for dispatchers. Also, as for the Command Support System for the State Medical Rescue, they set out principles of the system operation and the scope of responsibilities at different levels of the system administration. By the time those regulations came into force, there was a risk that emergency calls would not be handled properly. That could pose a threat to the health and life of high-risk patients.
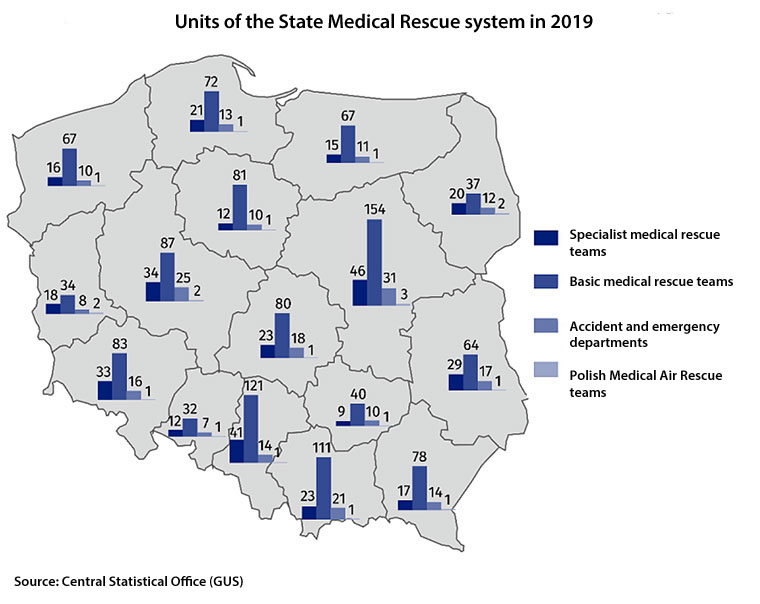
In 2019, as part of the State Medical Rescue System, there were 1577 medical rescue teams (369 specialist ones and 1208 basic ones). Also, the Polish Medical Air Rescue and medical personnel from 237 accident and emergency departments provided emergency medical care. 155 accident and emergency rooms and the total of 25 trauma centres cooperated with the State Medical Rescue System.
Command Support System for the State Medical Rescue
This is a standardised IT tool used by dispatchers, medical rescue team members and coordinators. It allows receiving emergency calls, managing medical rescue teams, registering medical occurrences, displaying their geolocation and tracking medical rescue teams. This is also a tool to monitor the quality of medical rescue system operation.
At the beginning of 2019, the Polish Medical Air Rescue was tasked with the system administration and development. That entity was not experienced in implementing such complex IT projects, though. As a result it could not meet the deadline and finish to implement the developed project by the end of 2020. The new deadline was scheduled for the end of 2022.
In 2018-2019, users of the Command Support System for the State Medical Rescue submitted critical comments on its operation, e.g.: there was no functionality enabling the update of ambulance routes on an ongoing basis, time on desktops and computer terminals was not synchronised which caused problems with handling emergency calls in proper order, the system stopped working when connected to a mobile terminal. Also, some errors occurred in the course of the system development with new functionalities, e.g. one could not log into the system, available medical rescue teams were not used and proper assessment of a patient’s consciousness could not be entered into the system. All that could threaten patients’ life or health.
Triage
Triage was practised in all the audited accident and emergency departments. An issue was related to different principles of the way triage was carried out in individual hospitals. That is why, a project was developed to standardise those principles: the Patient Support System for Accident and Emergency Departments (in Polish: TOP SOR). The system is to streamline the work of AEDs and thus help to shorten patient queues by redirecting low-risk patients to primary care.
The Minister of Health assigned the leading role in implementing the TOP SOR project to the Polish Medical Air Rescue. However, that entity made some errors at the stage of preparing the public procurement procedure. As a consequence, the tender was cancelled and the project implementation was postponed until 2021.
According to NIK, all that points to insufficient supervision of the Minister of Health over the system implementation. The need to launch TOP SOR seems to be even more urgent now considering that in 2019 low-risk AED patients made up from 29% to 69% (depending on data source). As a result, the waiting time of high-risk patients was increasing. NIK stands in a position that this situation results from limited access to primary and specialist care, as well as the absence of an effective mechanism limiting the provision of AED healthcare in the cases that did not need that.
Data and indicators
As a result of the said errors, delays and inconsistencies, the Minister of Health lacked access to reliable data about the quality of provided medical rescue services and the number of patients needing them. The data from the Command Support System for the State Medical Rescue, from provincial SMR action plans and from the National Health Fund were unreliable and inconsistent. It should be emphasised that access to reliable data is the preliminary condition for efficient system supervision. The absence of such data made it difficult for the Minister of Health to effectively refine the SMR system. Besides, the audits ordered by the Minister were lengthy and did not help improve the quality of medical rescue services.
Indicators of the SMR system operation include among others the median emergency response time and the maximum emergency response time. It is the governors’ responsibility to make sure the statutory parameters defining emergency response times are met. None of the audited provinces provided organisational conditions for medical rescue teams to reach the persons in need of urgent medical care in required time.
The median emergency response time laid out in the State Medical Rescue Act does not exceed 8 minutes in cities with more than 10 thousand inhabitants and 15 minutes outside those cities. As to the maximum emergency response time, it should be 15 minutes in cities with more than 10 thousand inhabitants and 20 minutes outside those cities. The percentage of medical rescue teams’ departures that did not meet that parameter in the total number of departures was more than 18% in 2017 and over 28% in 2018.
The emergency response times were observed only in case of incidents accompanied by sudden cardiac arrest.
Besides, in 3 of 5 audited provinces, 24-hour watch of medical rescue coordinators was not guaranteed (medical rescue coordinators are responsible for dispatchers’ cooperation; they are also to decide whether or not a patient should be admitted to hospital). The lack of the 24-hour watch in provincial hospitals was caused by the shortage of coordinators and could be dangerous for the health and life of patients who needed medical intervention.
Personnel shortage
Personnel shortage has been a long-time problem of the State Medical Rescue. In 2018, there were over 1 thousand emergency physicians, which - according to the national consultant in that area - covered only 39% of the demand for such specialists.
The deficit of physicians resulted in incomplete staffing of accident and emergency departments and medical rescue teams. Doctors working in AEDs were on duty for many hours, in extreme cases even up to 80 hours, without any rest. It happened that there was only one doctor on duty in an AED, not always an emergency physician. In some cases the position of an AED head remained vacant. Moreover, physicians in medical rescue teams worked, with only one-hour break, for up to 144 hours.
Apart from that, in some cases medical rescue teams were sent to patients without any physician. That was a breach of the provisions of healthcare contracts with the National Health Fund which ended in penalties imposed on hospitals. Because of the shortage of doctors in the system, those penalties failed to fulfil their preventive and disciplinary role.
Also the Polish Medical Air Rescue had problems hiring emergency physicians in 2018-2019. Low salaries resulted in high staff turnover. Nevertheless, constant readiness of air medical rescue teams to provide medical assistance in urgent cases was ensured.
According to NIK, personnel issues will probably get worse in the future. In the audited period, the number of physicians willing to specialise in emergency medicine declined. In 2018, training places in that specialty were used only in 14%, whereas in 2019 only in 10%. Corrective actions taken by the Minister of Health in 2018 also proved ineffective (he gave emergency physicians an opportunity to specialise in 14 other branches of medicine, using a ”short path”). Also the update of specialty training programmes did not solve the problem.
Expenditures
Despite an increase of expenditures in the audited period (by over 5% on accident and emergency departments and by 10% on medical rescue teams), those units still struggled with financial problems. All the audited hospitals had problems with covering (from funds received from the National Health Fund) the costs of operation of accident and emergency departments. The operation of AEDs generated even several millions’ losses for their hospitals.
NIK is of the opinion that the appointment of the Government Commissioner for State Medical Rescue in 2019 (fulfilling the role of the Secretary of State in the Ministry of Health at the same time) was a good step. His tasks include monitoring of actions, analysis of applicable provisions of law and existing solutions as well as preparation of proposals of new legal solutions to improve the operation of the State Medical Rescue.
Recommendations
NIK has addressed the following recommendations to the Minister of Health:
- to take effective steps to make sure the number of emergency physicians guarantees smooth operation of the SMR system;
- to ensure timely implementation of the development concept of the Command Support System for the State Medical Rescue and implement new functionalities in the system in a way that does not threaten proper SMR functioning;
- to strengthen supervision of the process of developing the TOPSOR system in a way guaranteeing its timely implementation;
- to structure the process of data creation and replacement in SMR system, critical to plan activities and supervise the system.
A system recommendation has been addressed to the President of the Council of Ministers:
- the Government Commissioner for State Medical Rescue should make a complex analysis of causes of the SMR system issues and prepare a comprehensive concept of the system development making sure the issues are solved. Also, permanent monitoring of the quality of medical rescue operation should be implemented.


